Socioeconomic inequalities in functional health in Chilean older adults

Old age is frequently marred by ill health. Socioeconomic conditions, too, play their part: the poorest also suffer from worse health conditions in Chile, as Pedro Olivares-Tirado and Rosendo Zanga Pizarro show, and arguably also elsewhere.
In the last three decades, Chile has experienced accelerated demographic ageing. In the 2017 Census, older adults (OA60+, aged 60 years and over) represented 16% of the country’s population, a share that is projected to increase to about 31% in 2050 (CELADE 2017). Population ageing raises the issue of the “quality of ageing” (Scott 2021), which may be significantly lowered by impairments in self-care, mobility, and cognitive functions affecting autonomy, independence and well-being in older persons. Different measures may be used to determine functional limitations. Regarding basic activities of daily living (BADL), six items are usually used: eating, bathing, personal mobility, toilet use, getting in/out of bed and dressing.
Socioeconomic inequalities and functional limitations
Functionality depends also on the social context in which older adults live and on their socioeconomic status, both of which affect their access to the healthcare system (Zhanget al 2019, Huang and Fu 2021).
Despite public policy improvements, Chile still has inequality in access, opportunity, quality, and financial coverage of health care, particularly among older adults (Fuentes-García et al 2013, Moreno et al. 2021). In a recent paper (Olivares-Tirado and Zanga Pizarro 2022), we examined the association between socioeconomic inequalities and functional limitations among Chilean older adults using self-reported BADL limitations and household income from the National Socioeconomic Characterization Survey-2017 (CASEN/2017).
Over 44,000 OA60+ were surveyed, 56% of them women. Most of them lived in urban areas, and had average schooling of 10.7 years for men and 9.3 years for women. The average adjusted household income was 1,638 US$ for men and 1,532 US$ for women. Furthermore, 85% of the OA60+ were covered by public health insurance, 7% by private health insurance, and the remaining were retired from the armed forces or had no insurance.
Table 1 shows the percentage of BADL limitations among OA60+, stratified by sex and severity. About 87% of men and 81% of OA60+ women had no BADL limitation. Concerning each BADL, personal mobility was the daily activity that showed the most significant functional limitations in both sexes, followed by bathing and dressing. In all BADLs, women presented more severe functional limitations than men.
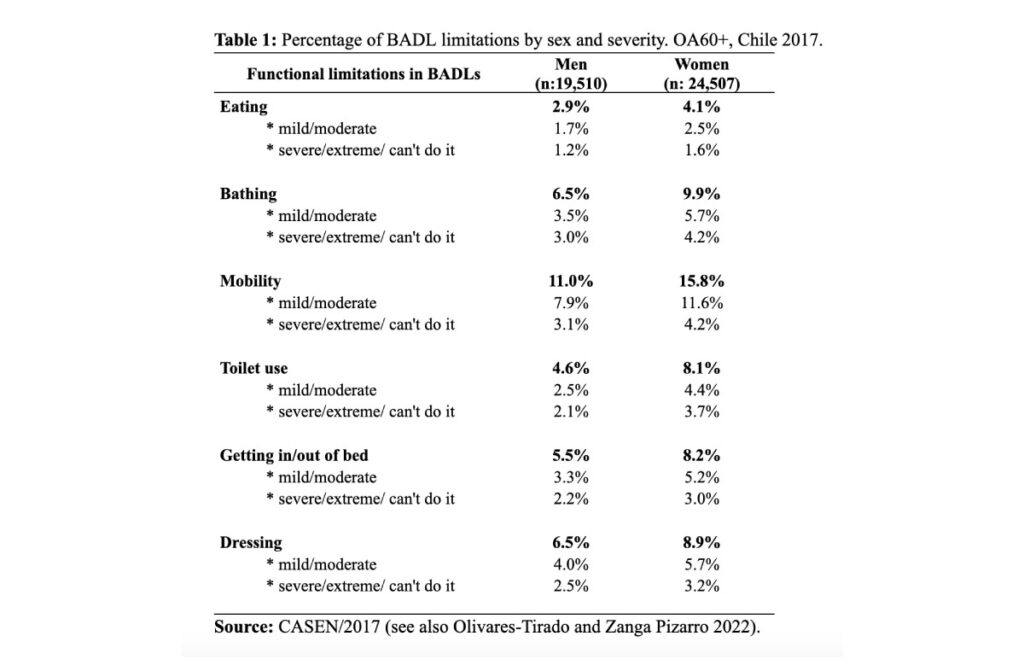
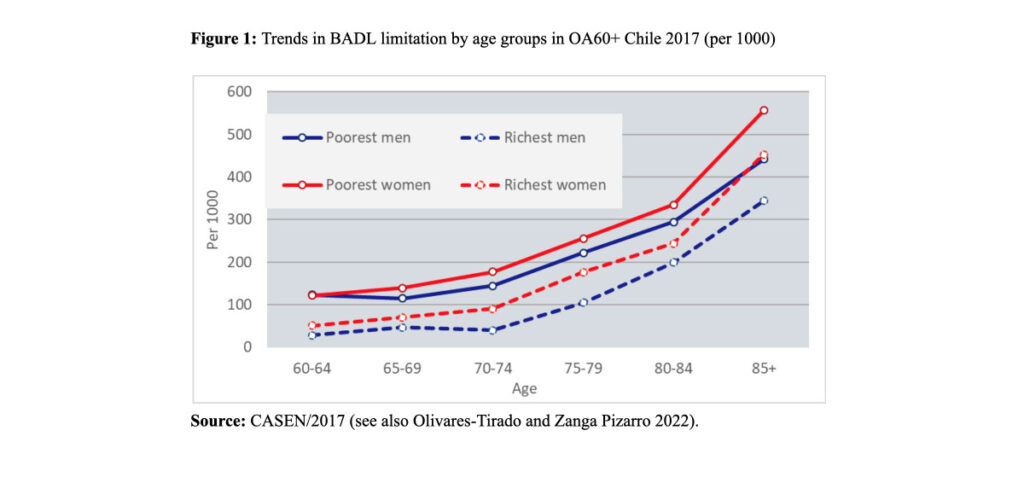
Figure 1 shows trends in BADL limitations of the poorest (first two deciles) and richest (last two deciles) OA60+ across age groups and by sex. An exponential increase in the frequency of BADL limitations across age groups in both sexes was observed. Women have higher prevalence (and higher severity) of BADL limitations than men in all age groups. The difference between the poorest and the wealthy decreases with advancing age.
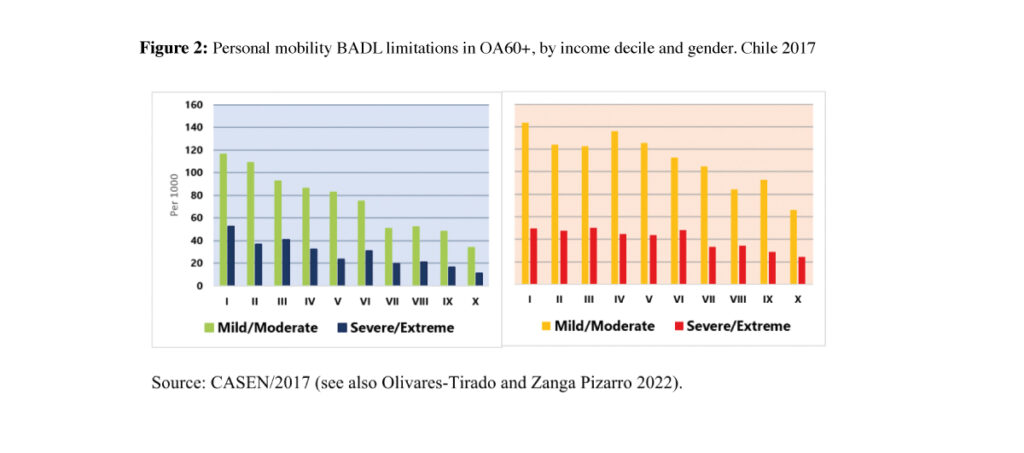
Let us consider the case of personal mobility limitation rates, for instance (other limitations have similar patterns, not shown here). Figure 2 shows the gradient of both severity levels, by gender and income decile, from the poorest (decile I) to the richest deciles (decile X). It emerges clearly that personal mobility limitations decline as income increases, and are always higher for women.
Policy implication of socioeconomic inequalities in functional health
While everybody is more likely to experience functional limitations as they age, significant gender and socioeconomic inequalities exist among Chilean older adults. Poor people present higher values in both severity levels of BADL limitations than rich people, and women are more affected than men.
These findings highlight the need for policies and programs to combat these socioeconomic inequalities in early adulthood in order to prevent and reduce limitations in functional health later in life. This goal will require significant changes in the social infrastructure and institutions around health, education, jobs, careers, pensions, legislation and community relationships.
The implication of living longer and achieving healthy ageing will inevitably place increased responsibility on the individual. The young generation most affected by increased longevity trends will require the most significant changes and adaptations in terms of education, careers, jobs and lifestyles.
References
CELADE. 2017. Long term population estimates and projections 1950-2100 Chile. 2017 Revision.
Fuentes-García A, Sánchez H, Lera L, Cea X, Albala C. 2013. Desigualdades socioeconómicas en el proceso de discapacidad en una cohorte de adultos mayores de Santiago de Chile. Gac Sanit. 27(3): 226–232.
Huang F, Fu P. 2021. Intergenerational support and subjective wellbeing among oldest-old in China: the moderating role of economic status. BMC Geriatr 21, 252. https://doi.org/10.1186/s12877-021-02204-y
Moreno X., Lera L., Moreno F. et al. 2021. Socioeconomic inequalities in life expectancy and disability-free life expectancy among Chilean older adults: evidence from a longitudinal study. BMC Geriatr 21, 176. https://doi.org/10.1186/s12877-021-02126-9.
Olivares-Tirado P, Zanga Pizarro. 2022. Socioeconomic Inequalities in Functional Health in Older Adults. Journal of Population Ageing 16(3). https://doi.org/10.1007/s12062-022-09404-3
Scott AJ. 2021. The longevity society. Lancet Healthy Longev. 2(12): e820-e827. doi: 10.1016/S2666-7568(21)00247-6.
Zhang CQ, Chung PK, Zhang R, Schüz B. 2019. Socioeconomic Inequalities in Older Adults’ Health: The Roles of Neighborhood and Individual-Level Psychosocial and Behavioral Resources. Front Public Health. 7:318. doi:10.3389/fpubh.2019.00318