Does health deterioration manifest at increasingly (dis)similar ages? Iñaki Permanyer, Francisco Villavicencio and Sergi Trias-Llimós explore inequalities in age-at-morbidity onset globally, and find these to be larger than lifespan inequalities. As longevity increases, the locus of health inequality is moving from death-related inequalities to disease- and disability-centered ones.
As longevity increases worldwide, are the ages at which individuals’ health deteriorates becoming increasingly concentrated over time, or more spread out? This is one of the fundamental questions around which the so-called ‘Compression vs Expansion of morbidity’ debate has revolved for a long time (Gruenberg 1977, Fries 1980), but whose answers have been mostly restricted to a small group of low-mortality countries. In a new study, we assess whether morbidity is compressing or expanding in all countries around the world (Permanyer, Villavicencio and Trias-Llimós 2023). We do so by estimating levels and trends of the newly proposed Healthy Lifespan Inequality (HLI) indicators (Permanyer et al. 2022), which measure the variability in the ages at which individuals cease to be in good health.
Longer and healthier lives enjoyed by everyone?
To investigate whether the ages at which individuals’ health deterioration becomes increasingly concentrated or dispersed over time, we use data from the Global Burden of Disease project (https://ghdx.healthdata.org/record/ihme-data/gbd-2019-life-tables-1950-2019) to calculate the so-called ‘age-at-morbidity onset distributions’ – which are used to estimate survival probabilities in good health. Variability is measured with the standard deviation, a popular indicator of the spread of a distribution.
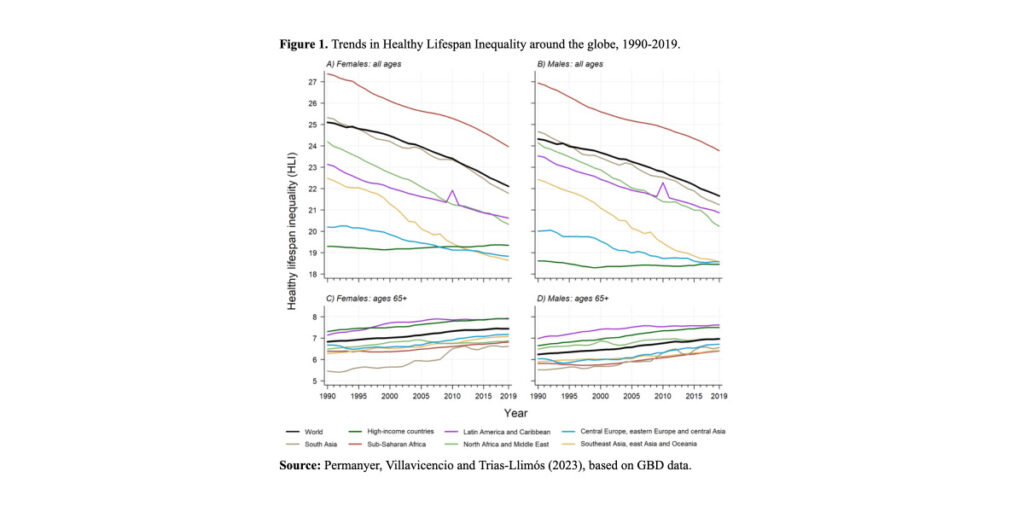
Figure 1, panels A and B, shows that the levels of HLI generally declined between 1990 and 2019 for both women and men, although not in high-income countries, where instead they stagnated. In general, females tend to exhibit higher variability in the ages at which they cease to be in good health. Another noteworthy exception is that of individuals aged 65 or more: in this group, the variability in age-at-morbidity onset has increased over time across all world regions (panels C and D in Figure 1).
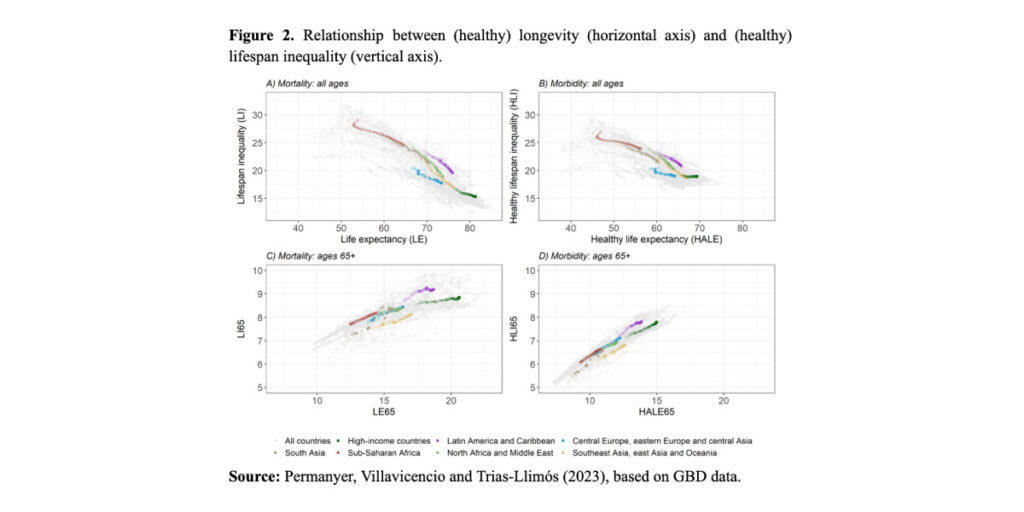
While the relationship between life expectancy and lifespan variability is strong and negative (Figure 2, panel A), the relationship between health-adjusted life expectancy and HLI is weaker and flatter (Figure 2, panel B). Among high-income countries and in Central Europe, Eastern Europe, and Central Asia, increases in health-adjusted life expectancy are not accompanied by reductions in HLI. Restricting the analysis to individuals above age 65, we observe a positive association between (healthy) longevity and (healthy) lifespan variability (Figure 2, panels C and D). This suggests that increases in healthy survivorship in those ages are associated with increases in the variability of the ages at which individuals’ health deteriorates, and similarly, increases in survivorship are associated with increases in the variability in age at death.
Discussion and implications
Previous approaches to assess whether morbidity is compressing or expanding have relied on the comparison of average indicators (i.e., average longevity, or life expectancy, versus average healthy longevity, or health-adjusted life expectancy). However, such average-based approaches do not take into consideration the variability in individuals’ health deterioration processes – a fundamental ingredient that, according to Fries (1980), should be included when studying morbidity dynamics, and which was incorporated in our analyses. Preliminary calculations suggest that the different approaches to assess whether morbidity is compressing or expanding do not yield consistent results, an issue not discussed here and that deserves further investigation.
Overall, high-mortality countries have been successful in increasing (healthy) longevity while simultaneously reducing (healthy) lifespan inequality. This has been the case of sub-Saharan Africa, South Asia, North Africa and the Middle East, or other regions with plenty of room for improvement. Conversely, low-mortality countries have not been very successful in further reducing the variability in healthy lifespans, so it is not clear whether morbidity is compressing or expanding there. Such stagnation might be the result of forces pushing in opposite directions. On the one hand, increases in living standards or the adoption of healthier lifestyles can postpone the deterioration of individuals’ health. On the other hand, screening and prevention programs could lower the age at diagnosis of important diseases (like mental disorders or cancers). Lastly, existing and broadening socioeconomic inequalities can contribute to widening the distribution of ages at which morbidity starts affecting individuals’ health.
The variability in the ages at which morbidity starts can be much larger than the variability in the ages at which individuals die, and this difference increases over time. While age at death is becoming increasingly predictable in longevity vanguard countries, the age at which health starts deteriorating is as uncertain now as it used to be three decades ago – an important finding with consequences for planners aiming to reduce population health inequalities. For instance, retirement or health care policies exclusively based on (increasing) trends in life expectancy might miss the mark and have deleterious social consequences if the corresponding morbidity onset distribution widens over time.
Interestingly, the same living standard improvements, medical innovations and technological breakthroughs that have contributed to reducing mortality-related inequalities across the world (as reflected in the decreasing inequalities in basic survival indicators like life expectancy at birth) have in turn contributed to the emergence of new layers of morbidity-related inequalities among adults at older ages, often to the advantage of privileged countries or socioeconomic groups. Our results point towards a compositional shift in health inequalities within countries: as longevity increases worldwide, the locus of health inequality over the lifespan is gradually moving from death-related inequalities to disease- and disability-centered ones. This compositional shift in health inequality should be taken into consideration in the elaboration of prospective public health policies.
References
Fries JF. (1980), “Aging, natural death, and the compression of morbidity”, New England Journal of Medicine 303:130–5.
Gruenberg EM. (1977), “The failures of success”. Milbank Mem Fund Q Health Soc: 3–24.
Permanyer, I., Spijker, J. and Blanes, A. (2022), “On the measurement of healthy lifespan inequality”, Population Health Metrics 20, 1. https://doi.org/10.1186/s12963-021-00279-8
Permanyer, I., Villavicencio, F. and Trias-Llimós, S. (2023), “Healthy lifespan inequality: morbidity compression from a global perspective”, European Journal of Epidemiology, DOI: 10.1007/s10654-023-00989-3.