Innovations in register data: the value of linkages to prescription databases illustrated by an analysis of underuse of medication among the unmarried

Data from registers that cover entire national populations have been extensively used in demography, other social sciences, and epidemiology over the last three decades.
The Nordic countries in particular have very valuable registers which, under certain restrictions, can be linked to one another. They include information about demographic events (births, deaths, marriages, divorces, immigration, emigration and internal migration), health (e.g. birth abnormalities, anthropometric measures for conscripts, cancer cases), skills (e.g. school grades, cognitive tests for conscripts), and socioeconomic factors (e.g. education, labour income, various types of allowances). Because this information extends many years back in time, there is a good potential for longitudinal analysis. It is also possible to take into account similar information about spouses, parents and children, as well as people living in the same municipality or smaller aggregate units. Additional information about place of residence can be added from other sources to further enrich a multilevel study. Whereas the menu of variables may not be quite as impressive as in some surveys (lacking, for example, information about attitudes, expectations, and health related behaviours), there are three large advantages associated with the use of register data: very little misreporting, no sample bias, and large data sets which allow detailed analyses that would otherwise be impossible.
Databases of prescriptions in Nordic countries
In all Nordic countries, one of the newest additions to the registers are prescription databases, which include all purchases of prescription medicine, except those made by the institutionalized population (Furu et al. 2011). People who purchase medicine typically use it either for preventive purposes (e.g. statins to prevent heart diseases for those with a high cholesterol level), or as part of a treatment. Some medicines are used for multiple pathologies; others for one specific disease and are therefore good indicators of this disease. Researchers may, for example, use the sum of all different medicines purchased within a certain period as a proxy for general health, or select certain medicines as indicators of specific diseases or group of diseases (Kuo et al. 2011). Prescription databases linked to other registers are therefore potentially very useful to demographers interested in health issues.
On the negative side, however, use of prescription medication is not a perfect indicator of morbidity as it is influenced by individuals’ consulting behaviour and the prescribing behaviour of doctors, as well as by the presence of a particular medical condition. Medication data must therefore be used very cautiously. Three types of use stand out as particularly promising for demographers and health researchers. First, if some individuals purchase more medicines than others, this may be taken as an indication that the former have poorer health if there is little reason to expect a corresponding variation in the use of health care and thus the chance of being diagnosed and getting a prescription. As a special case of this, there are some diseases, such as diabetes among the young (Type I), that have a generally very high chance of being diagnosed. Second, and similarly, one may learn something about determinants of health by studying changes in purchases over part of a person’s life course, provided that there is not a corresponding change in health care use over time for that person. (Using such a longitudinal procedure, one also controls for unobserved characteristics of the individual that are time-invariant, and that with other study designs might confound observed relationships between health and the potential health determinant under consideration). Third, one may compare medication purchases with data on other good indicators of health to learn about differences in health care use.
An example of the use of the Norwegian Prescription Database
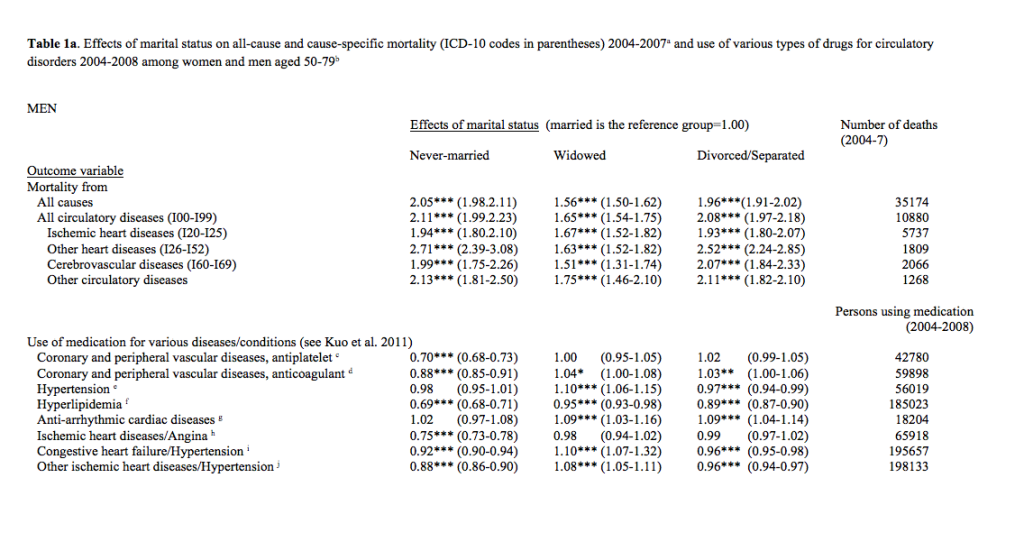
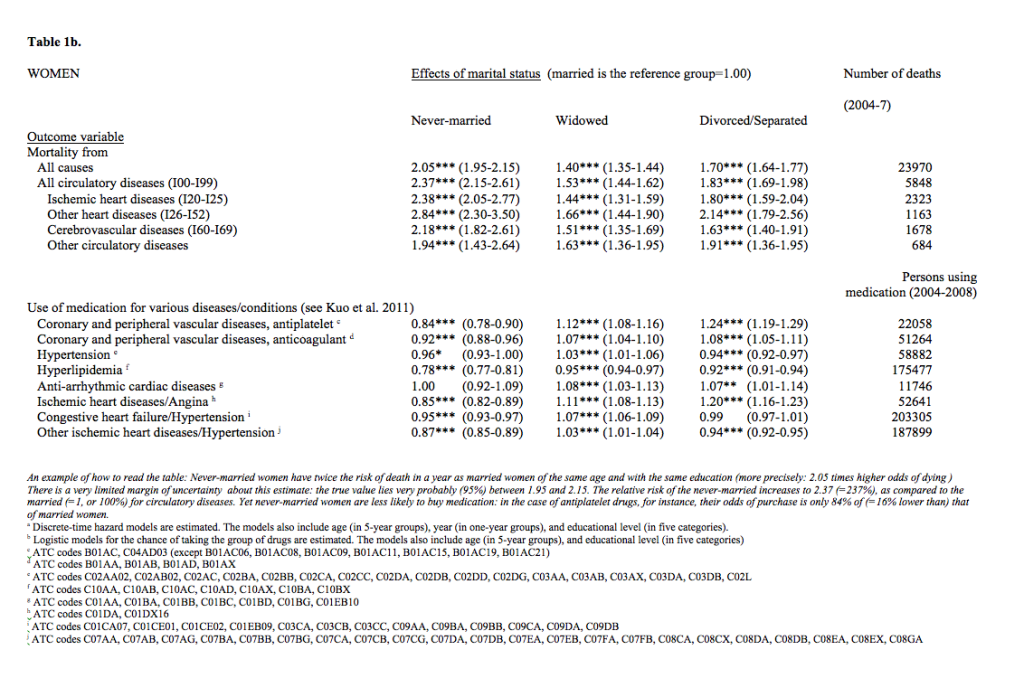
In a study of the latter type, we used data from the Norwegian Prescription Database (started in 2004) and some other registers to estimate various types of models for the purchase of medicine for eight circulatory conditions by people aged 50-79 during 2004-2008 (for details, see Kravdal and Grundy 2014). Differences in medication purchase by marital status were compared with differentials in circulatory disease mortality during 2004-2007. We found that the unmarried had 1.4-2.8 times higher mortality from the four types of circulatory diseases considered (see Table 1), which fits with patterns reported elsewhere. The most plausible interpretation of this – which is also supported by a few survey-based studies of the prevalence of circulatory conditions from other countries – is that the unmarried have a larger burden of such diseases, which implies that they need more medication. Yet, our results showed that they purchased either less or only slightly more medication for these diseases and their risk factors (see Table 1). Use among the never-married was particularly low, largely reflecting a low chance of making a first purchase (not shown in the table).
These results suggest that the unmarried, and especially the never-married, to a larger extent than the married, have circulatory disorders that are undiagnosed or for which they for other reasons underuse medication. Inadequate use of these potentially very effective drugs in such a large population group would, of course, represent a serious public health challenge, so further research is needed to shed light on this phenomenon.
This finding, made possible by the new type of register data, may provide a partial explanation for the increasing marital status differences in all-cause mortality and mortality from circulatory diseases observed in several countries, despite the rising prevalence of consensual unions among the unmarried. The gap between the married and the never-married has increased the most. Possibly, one reason for the growing excess mortality among the never-married is that they are especially likely to underuse medication for circulatory disorders, and that the resulting health disadvantage due to this has increased in step with the introduction of new medicines which have contributed greatly to the general reduction in mortality from such diseases (Ford et al., 2007; O’Flaherty et al., 2013).
References:
Ford, E.S., Ajani, U.A., Croft, J.B., Critchley, J.A., Labarthe, D.R., Kottke, T.E., et al. (2007). Explaining the decrease in U.S. deaths from coronary disease, 1980-2000. New England Journal of Medicine, 356, 2388–2398.
Furu, K., Wettermark, B., Andersen, M., Martikainen, J.E, Almarsdottir, A.B., & Sørensen, H.T.(2011). The Nordic countries as a cohort for pharmacoepidemiological research. Basic & Clinical Pharmacology & Toxicology, 106, 86-94.
Kuo, R.N., Dong, Y.-H., Liu, J.-P., Chang, C.-H., Shau, W.-Y., & Lai, M.-S.(2011). Predicting healthcare utilization using a pharmacy-based metric with the WHO’s Anatomical Therapeutic Chemical Algorithm. Medical Care, 49, 1031-1039.
Kravdal, Ø. & Grundy E. (2014). Underuse of medication for circulatory disorders among unmarried women and men in Norway. BMC Pharmacology and Toxicology 15:65.
O’Flaherty, M., Buchan, I., & Capewell. (2013). Contributions of treatment and lifestyle to declining CVD mortality: why have CVD mortality rates declined so much since the 1960s? Heart, 99, 159-162.