Infectious diseases in ageing populations: a neglected cause of mortality?

In countries with high life expectancies, death is predominantly the consequence of cancers and diseases of the circulatory system. Yet, infectious diseases have not disappeared from public health concerns, and the fear of new epidemics re-emerges from time to time (e.g. HIV, influenza A pandemics, and Ebola epidemics). In this regard, attention has mainly focused on the combined roles of environmental change, socio-economic organization and human behaviour in the circulation of infectious agents (Suk and Semenza 2011). But another vector of resurgence of infectious diseases, namely population ageing, has been largely overlooked. As early as 1982, Manton and Stallard foresaw that population ageing might result in a “fresh upsurge in infectious diseases”. Older people are not necessarily the prime victims of epidemics, but old age is a risk factor: immuno-senescence as well as other age-associated anatomical and physiological modifications increase susceptibility to infections that are frequently more severe and more difficult to treat (Gavazzi and Krause 2002).
What is an infectious disease?
The question may seem trivial but it is not. Publicly available figures are usually based on the infectious and parasitic diseases listed in the first chapter of the International Classification of Diseases (ICD). This chapter, called “certain infectious and parasitic diseases”, contains only infectious diseases that cannot be classified under a given anatomic site. For example, influenza and pneumonia are classified with the diseases of the respiratory system, peritonitis with the diseases of the digestive system, urinary tract infection with the diseases of the genitourinary system, etc. There is no internationally validated list of infectious diseases. In our study (Désesquelles et al., 2015), in addition to the aforementioned chapter (“certain infectious and parasitic diseases”), we selected all infectious diseases classified elsewhere in the 10th ICD. We included all subcategories containing one of these terms: infection, infectious agent, abscess, gangrene and fever. Diseases that in most cases have an infectious origin (e.g. some inflammatory diseases such as endocarditis) were also included.
Infectious diseases can kill you in several ways
Cause-of-death statistics usually concern the so-called “underlying cause” of the death. According to the World Health Organization (WHO), the underlying cause is the disease that initiated the train of events leading to death. Of course an infectious disease can be the underlying cause of a death. But infectious diseases often contribute to death in other ways. They may be a consequence or a complication of the underlying cause (e.g. fall resulting in bed confinement and pneumonitis) or its treatment (e.g. immunosuppression due to chemotherapy resulting in septicaemia). Infectious diseases may be a risk factor for the underlying cause (e.g. chronic viral hepatitis for liver cancer). Lastly, they may play the role of a “background factor” (Manton and Stallard 1982): when combined with the underlying cause, the risk of dying is increased. Typically, chronic infections such as HIV or hepatitis may play such a role. So in a number of cases, infectious diseases will not be identified as the underlying cause of death. Hence, to correctly estimate their contribution to mortality, all causes (underlying or contributing causes, also called multiple causes) reported on a death certificate need to be taken into account (Désesquelles et al. 2012).
In France and Italy, infectious diseases contribute to about 20% of deaths at ages 65 and over
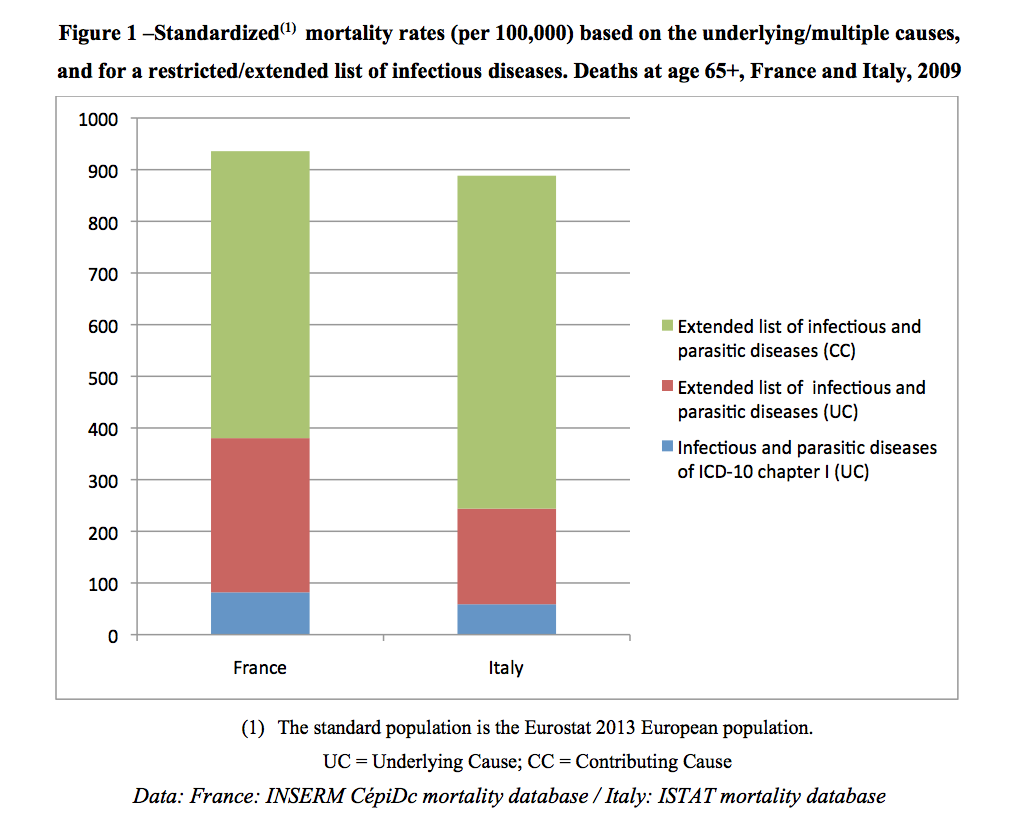
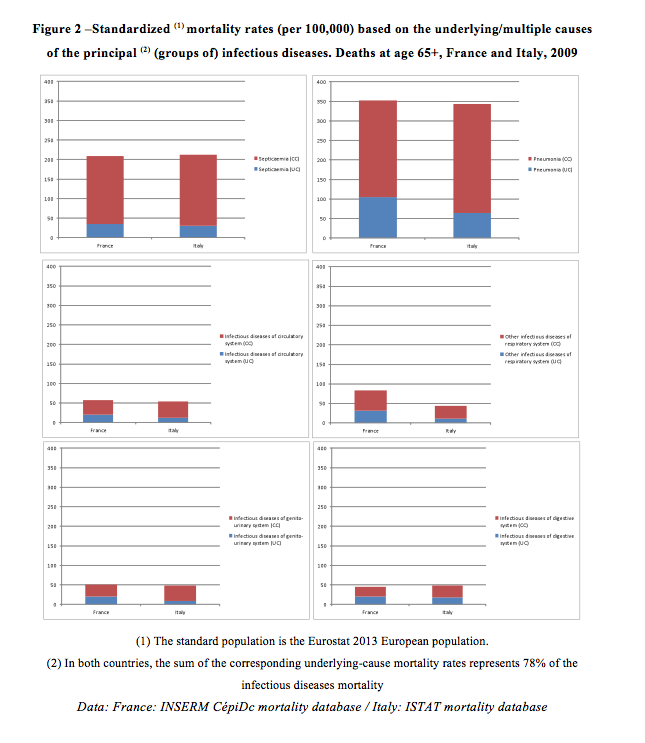
Let us consider the cases of France and Italy. In 2009¹, among over-65s, 8,600 deaths in France and 7,000 deaths in Italy were attributed to an infectious disease as defined by the first chapter of the ICD. Using our “extended list of underlying causes”, the numbers rose to 31,296 in France and 21,296 in Italy. The corresponding underlying-cause mortality rates were thus multiplied by 3.6 in France and 3.1 in Italy (Figure 1). In both countries, half of the observed increase was due to pneumonia.
When all causes reported on the death certificate were considered, the number of deaths involving an infectious disease either as underlying or contributing cause increased to 88,696 in France and 95,506 in Italy. The multiple-cause mortality rates of most (groups of) infectious diseases were twice the underlying-cause mortality rate (Figure 2). The ratio was especially high for septicaemia (6.0 in France and 7.1 in Italy). In other words, more than five in six entries of septicaemia on death certificates were not the underlying cause of the death. In France, the share of deaths from an infectious or parasitic disease at ages 65 and over increased from 2.1% to 7.3% when the extended list was used and to 20.8% when the contributing causes were also considered. For Italy, these percentages were 1.4%, 4.2% and 18.7%, respectively.
A global issue for health policies
In 2015 the number of deaths increased in several European countries, probably as a result of severe influenza epidemics (Caltabiano 2015). Our research shows that in ageing populations, infectious diseases represent a far larger, latent share of the cause-of-death profile than might be assumed. This observation suggests that a number of actions are needed. Some are not specific to older age groups, though they may be adapted to its characteristics (e.g. actions aiming at limiting antimicrobial resistance through good prescription strategies and improved treatment adherence). Others are more specific, such as actions to limit the spread of infections in institutional settings or research on the senescence-related mechanisms of immunosuppression.
The issue we raise here is not limited to the older populations of high-income countries. Firstly, the fight against infectious diseases has no boundaries. Secondly, low- and middle-income countries (LMICs) are now confronted with a dual burden of both communicable and non-communicable diseases (Remais et al. 2013). So, the interactions between these two types of diseases and the development of combined strategies to prevent and cure them are of concern to LMICs as well.
References
Caltabiano M (2015) L’eccesso di mortalità del 2015: alcuni dati su cui riflettere. Neodemos.
Désesquelles A., Salvatore M.A., Pappagallo M., Frova L., Pace M., Meslé F., Egidi V. (2012) Analysing multiple causes of death: which methods for which data? An application to the cancer-related mortality of France and Italy. European Journal of Population, 28 (4):467-498.
Désesquelles A., Demuru E., Pappagallo M., Frova L., Meslé F., Egidi V. (2015). After the epidemiologic transition: a reassessment of mortality from infectious diseases among over-65s in France and Italy. Int J Public Health, 60: 961-967
Gavazzi G, Krause KH. (2002) Ageing and infection. Lancet Infect Dis 2(11): 659-666.
Manton KG, Stallard E. (1982) Temporal trends in U. S. multiple cause of death mortality data: 1968 to 1977. Demography 19: 527-547.
Remais JV, Zeng G, Li G, Tian L, Engelgau MM. (2013) Convergence of non-communicable and infectious diseases in low- and middle-income countries. Int J Epidemiol 42(1):221-7.
Suk JE, Semenza JC. (2011) Future infectious disease threats to Europe. Am J Public Health 101(11): 2068-2079.
Footnote
¹Latest available data when we wrote our paper (Désesquelles et al. 2015). More recent data have now been published in both countries, which we have not yet analysed.