From deprivation to neonatal and post-neonatal mortality in Bolivia

Filippo Temporin identifies three possible mechanisms whereby deprivation can affect neonatal and post-neonatal mortality. Using data from the 2008 Bolivia Demographic and Health Survey, however, he concludes that in a context of widespread poverty, community-level absolute deprivation is the only significant predictor of infant mortality.
Introduction
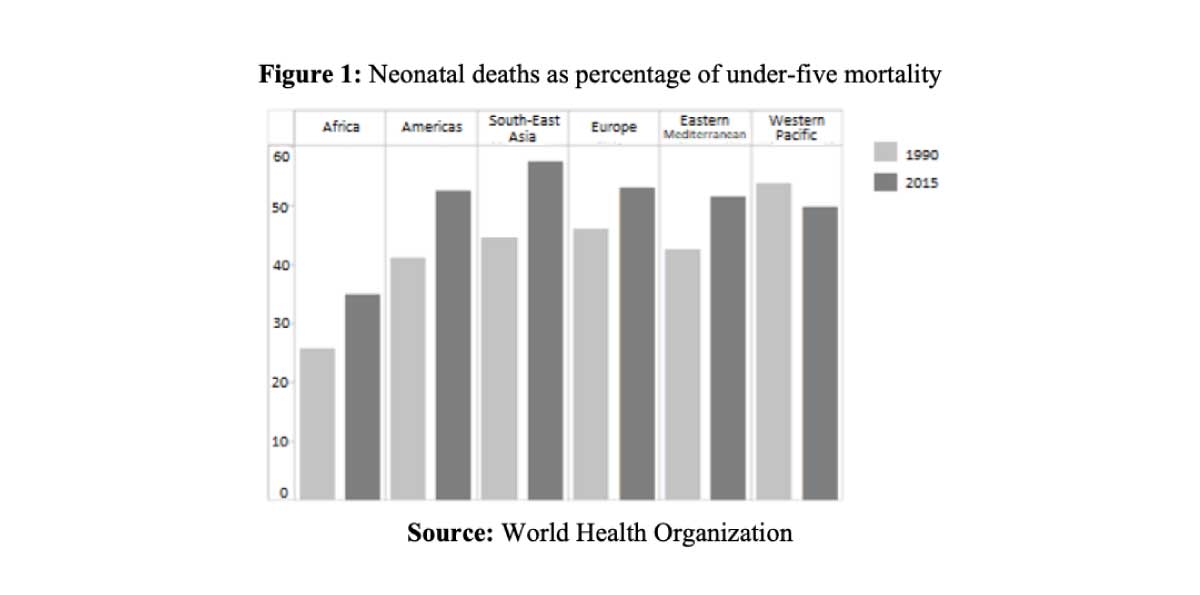
The reduction of child mortality represents a major challenge for health systems worldwide, especially in its neonatal and post-neonatal components (first 28 days of life; 29th day of life to first birthday, respectively). Although neonatal mortality rates have decreased over the last decades, the pace of decline has been slower than that of infant mortality (age 0-12 months) and child mortality (age 0-4 years, or “under 5”). As a result, neonatal mortality has accounted for a gradually higher proportion of under-five mortality, from 40% of the total in 1990 to 47% in 2019, according to UNICEF data. Figure 1 shows that this pattern has occurred in every area of the world, except in the Western Pacific.
This trend might be explained, among other factors, by a differential effect of neonatal and post-neonatal determinants. However, the patterns of association between socioeconomic factors and mortality occurring in the neonatal period have been studied less than in subsequent periods of life (Neal, 2009).
In my analysis (Temporin 2020), the main determinant of interest is deprivation, interpreted as a lack of resources to satisfy basic needs related to housing conditions and living standards. This composite variable includes indicators of access to a mains power supply, access to clean water, type of sanitation, floor material, type of cooking fuels, and refrigerator ownership.
The literature suggests that deprivation may affect mortality through three mechanisms:
- absolute deprivation (average level of deprivation in a community): absolute deprivation can be a determinant of mortality, due, among other factors, to indoor air pollution and inadequate water quality and sanitation (Johannesson 2004);
- relative deprivation (difference between each household’s level of deprivation and the average of their community): being more deprived than the reference group average can affect mortality by generating stress-induced behaviours and eroding social cohesion; associations between unfavourable social comparisons and negative health outcomes have been found in the US (Lhila and Simon 2010);
- deprivation inequality (degree of dispersion of deprivation within a community): the contextual effect of the variation in deprivation within communities can determine negative health outcomes, and inequality can be a hazard for the whole population rather than just for those with less favourable social comparisons (Wilkinson 1997).
Using data from the 2008 Bolivian Demographic and Health Survey, my analysis aimed to assess the different patterns of association between these mechanisms and neonatal and post-neonatal mortality in Bolivia.
The Bolivian context
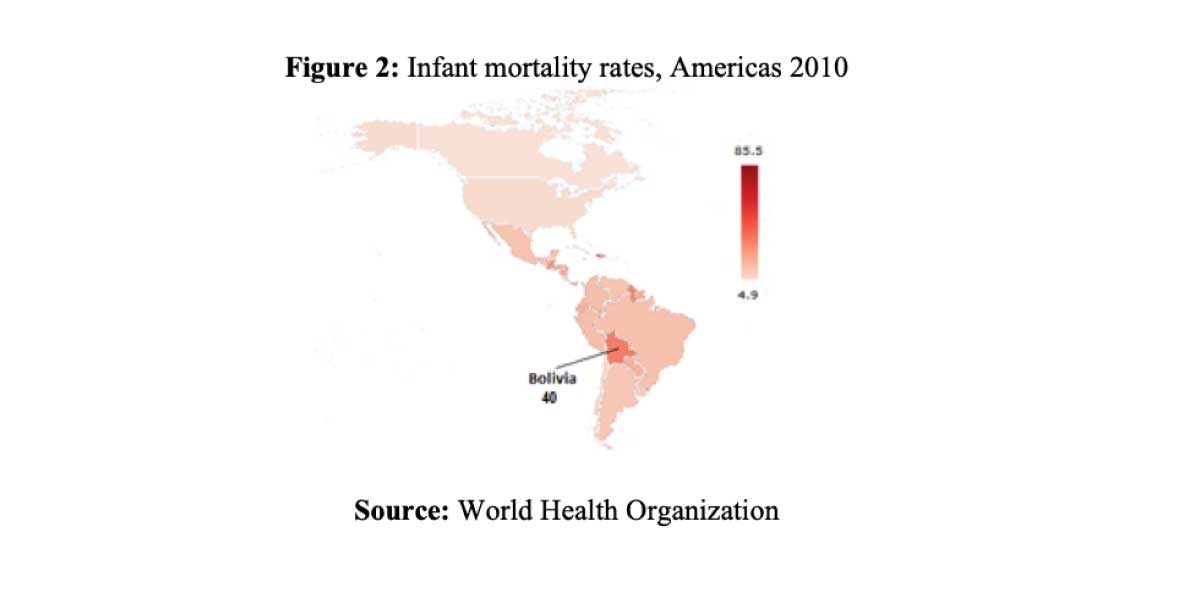
Ten years ago, Bolivia was a laggard in the demographic transition in the Americas (Figure 2). According to World Bank data, Bolivian neonatal, infant, and under-5 mortality rates were among the highest in the continent—at, respectively, 23, 37, and 47 deaths per 1,000 live births, compared with averages of 12, 19 and 23 deaths per 1,000 live births, respectively, in Latin America as a whole that same year. Moreover, in 2008, Bolivia was one of the most unequal and poorest countries in South America, with widespread chronic malnutrition and one of the continent’s highest poverty headcount ratios. There was marked urban-rural inequality in the distribution of wealth and in the demographic indicators of early-age mortality. Bolivia was also characterized by a large indigenous population, accounting for more than 60% of the total, who were affected by social exclusion in terms of poverty, education, and health (Coa and Ochoa, 2009).
In recent years, positive trends in the mortality-related indicators have been observed, and Bolivia has converged with the rest of the continent: according to World Bank data, Bolivian neonatal, infant, and under-5 mortality rates were respectively 15, 21 and 26 deaths per 1,000 live births in 2019. This positive trend can be imputed, at least in part, to the Bolivian health reform. Launched in 1996, it was revived in 2002, with the implementation of a package of free services targeting childbirth and infant and maternal health. Moreover, thanks to redistribution programmes, the overall level of poverty declined (35% of the population below the national poverty line in 2018, compared to 57% in 2008), and the Gini index is estimated to have dropped from 0.51 in 2008 to 0.42 in 2018.
Results and discussion
The three variables of interest in my analysis were absolute deprivation, relative deprivation and deprivation inequality at community level, i.e. among clusters of households within a geographical living environment.
After controlling for several biodemographic variables (e.g. birth order and maternal age at birth) and socioeconomic variables (e.g. parents’ occupation and education), community-level absolute deprivation was the only observed variable significantly associated with neonatal and post-neonatal mortality (Table 1; borderline p-value for the post-neonatal period). While it is impossible to decompose the role of each measure of deprivation in these models, the literature suggests that environmental factors linked, among others, to water quality and sanitation and access to mains electricity are a major determinant of infant health (De Graaf et al., 2013). In these models, neonatal mortality appears to be more closely associated with community-level deprivation than post-neonatal mortality: in fact, environmental factors play a role not only in newborns’ health, but also on their mothers’ health throughout pregnancy.
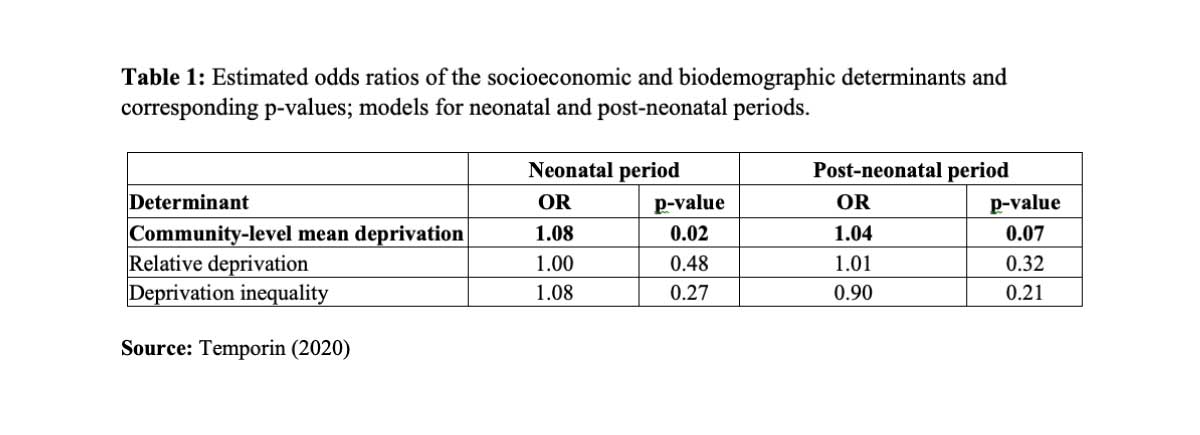
The other determinants of interest are not significantly associated with the mortality outcomes. The pathways linking relative deprivation and deprivation inequality to mortality, like maternal stress-induced smoking and poor quality of social life, found no support in this study. However, inequality in the distribution of deprivation might nonetheless affect health outcomes in more unequal contexts than Bolivian communities in which wealth tends to be distributed homogeneously.
To conclude…
The main finding of this analysis is that in contexts of widespread poverty and deprivation like Bolivia, satisfying the basic needs of everyday life is more important than wealth distribution inequalities in determining infant health outcomes; relative deprivation and inequality may play a role in mortality only after basic needs are met. The improvement in Bolivian living standards over the last decade is likely to have played a fundamental role in the recent decline in infant mortality, especially with respect to its neonatal component.
Government and local authorities have a major role to play in tackling neonatal and overall infant mortality in contexts where absolute deprivation is still a reality. Programs aimed at improving community-level factors, such as extending the power grid and enhancing latrine facilities and domestic water supply, represent a crucial step in this direction.
References
Coa, R., & Ochoa, L. H. (2009). Bolivia 2008: Results from the Demographic and Health Survey. Studies in Family Planning, 41, 301–306.
De Graaf, J. P., Ravelli, A. C., de Haan, M. A., Steegers, E. A., & Bonsel, G. J. (2013). Living in deprived urban districts increases perinatal health inequalities. Journal of Maternal-Fetal & Neonatal Medicine, 26, 473–481.
Johannesson, M. (2004). Absolute income, relative income, income inequality, and mortality. Journal of Human Resources, 39, 228–247.
Lhila, A., & Simon, K. I. (2010). Relative deprivation and child health in the USA. Social Science &
Medicine, 71, 777–785.
Neal, S. E. (2009). Neonatal mortality in developing countries: An analysis of trends and determinants (Doctoral dissertation). School of Social Sciences, University of Southampton, Southamptom, UK.
Temporin, F. (2020). How Does Deprivation Affect Early-Age Mortality? Patterns of Socioeconomic Determinants of Neonatal and Postneonatal Mortality in Bolivia. Demography, 57, 1681–1704
Wilkinson, R. G. (1997). Socioeconomic determinants of health: Health inequalities: Relative or absolute material standards? BMJ, 314, 591–595.