Besides its morbidity and mortality effects, COVID-19 gave rise to several non-pharmaceutical policy interventions affecting citizens’ social and economic conditions. Veronica Toffolutti et al. find that these measures negatively affected mental well-being in 28 European countries, and particularly so among groups with already alarming pre-pandemic levels of mental well-being, such as women and individuals living with young children.
COVID-19, policy interventions and mental well-being
The European Union (EU) and the UK have been hit hard by the COVID‒19 pandemic. Besides causing disease and death, COVID‒19 generated a “parallel epidemic of poor mental health”, whose effects could linger long after the pandemic has subsided (WHO, 2021; Santomauro et al., 2021).
Pandemic-related distress can depend on several factors, including fear of illness and uncertainty about the impact of the crisis (Moreno et al., 2020). It is also a result of economic hardship, family tensions, social isolation, and perceived limitations of freedom and interaction with others, caused, for example, by the physical distancing measures implemented to contain the pandemic (e.g. stay-at-home requirements and school closures) and health-related interventions (e.g. testing and contact tracing). The latter measures might have also accentuated people’s fears of illness, in the same way that income-support and debt-relief policies raised fears of economic uncertainty (Moreno et al., 2020).
To what extent did these policies affect citizens’ mental well-being? And were specific groups affected more than others? For instance, women and individuals residing with young children may have suffered more, as physical distancing disrupted childcare arrangements and increased childcare workload (Douglas et al., 2020).
Mental well-being among Europeans
To answer these questions, in a recent study we used the first three waves of the Eurofound e-survey “Living, Working and COVID‒19” conducted between April 2020 and March 2021, covering 15,147 individuals observed at least twice in the 27 EU member states and the UK (Toffolutti et al., 2022; Eurofound, 2020). We matched these individual-level data, including respondents’ mental well-being (measured by the WHO‒5 index ranging between 0 and 25), with data on policy implementation in their country of residence at the time of interview, taken from the Oxford COVID‒19 Government Response Tracker (Hale et al., 2020).
Table 1 provides descriptive statistics on mental well-being by societal groups. It suggests a clear socio-economic gradient. Men, people with a tertiary-degree, those living with a partner, and those not living with children report higher levels of mental well-being on average.
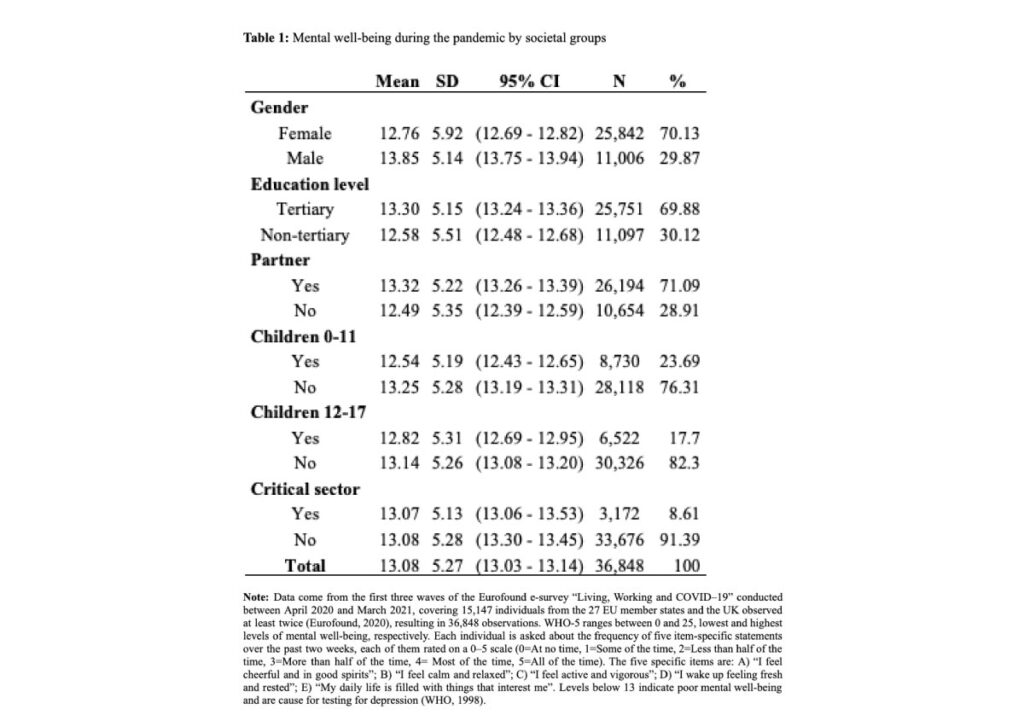
To grasp how much mental well-being changed during the pandemic, we estimated the average WHO-5 score from the European Quality of Life Survey in 2016 for the same 28 countries (Eurofound, 2016), reweighting the data to reflect our sample’s structure by country and gender. Overall, mental well-being significantly declined between 2016 and 2020-21, during the pandemic, from 16.16 down to 13.08.
Women’s mental well-being was already considerably lower than men’s in 2016: 15.91 versus 16.77 points (not in Table 1). And while both genders experienced a decline during the pandemic, the gender gap widened, from 0.86 in 2016 to 1.09 in 2020-21.
Differences in the association between policies and mental well-being across key groups
To assess the association of government interventions with individuals’ mental well-being within and between different key groups in society, we estimated multivariate regression models controlling for daily COVID‒19 cases and deaths, monthly unemployment rates, country and wave fixed-effects, and individual random-effects. Figure 1 presents the main results graphically. The estimated coefficients represent the average point difference in the mental well-being of individuals interviewed during implementation of the policies (with an average exposure time of 115 days for them) with respect to that of individuals having similar characteristics but interviewed just before enforcement of the policies or after they had been lifted (42 days before, on average). We compute the results by gender, educational attainment, and work typology (red circles represent workers in a critical sector, i.e. sectors that provide essential services such as healthcare or agriculture that cannot be interrupted; blue circles represent other workers) as well as differences between the groups (green triangles).
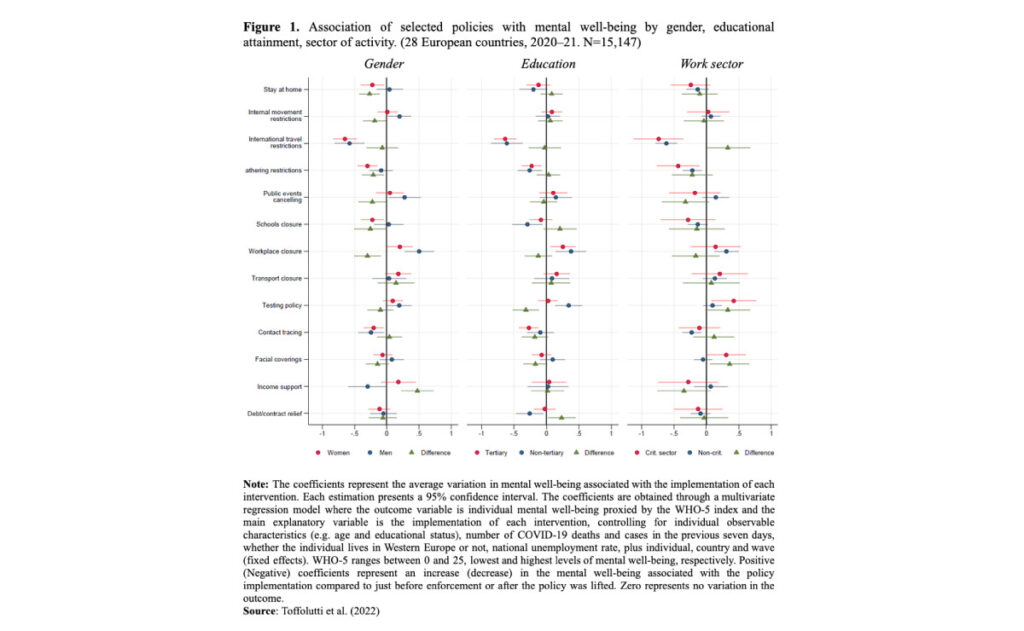
Women fared worse than men in terms of mental well-being under stay-at-home requirements, internal movement restrictions, restrictions on private gatherings, cancellation of public events, school closures, and workplace closures. These policies were negatively associated only with women’s mental well-being, except for workplace closures which were related positively with mental well-being of both genders, though with a larger magnitude for men. Only for income support did women fare better than men. The largest (negative) association was found for international travel restrictions for all the groups analysed here.
Differences between tertiary and non-tertiary educated were found for testing policies, for which the tertiary educated fared less well than the lower educated, and contract or debt relief policies, for which they fared better.
In the comparison between critical-sector and other workers, the former fared better under facial coverings policies.
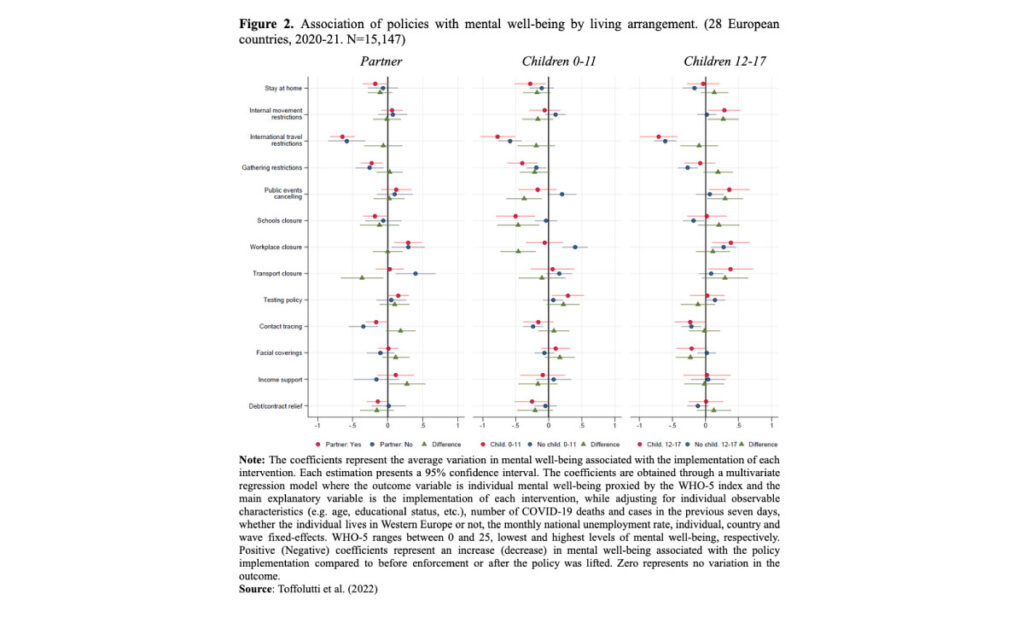
Figure 2 presents the results with respect to living arrangements, i.e. cohabiting versus not, living with or without children aged below 12 years, and living with or without children aged 12-17 years.
The mental well-being of those not living with a partner improved in association with public transport closures, but slightly worsened following income support measures.
Not surprisingly, those living with children younger than 12 suffered more than others from the cancellations of public events, school closures, and benefitted less from workplace closures.
Individuals living with children aged between 12 and 17 years (Figure 2, column 3), fared better with respect to internal movement restrictions and public events cancellation.
Implications
These relationships may have important policy implications for three main reasons. First, our estimates are likely conservative, as they are based only on data collected during the first pandemic year, and thus do not capture the full variation in mental well-being caused by the first implementation of COVID-related interventions.
Second, our results document an exacerbation of the differences in mental well-being that existed before the pandemic. For instance, women’s mental well-being before the pandemic was already lower than men’s, and the gap widened with the pandemic. Policy measures may have contributed to this, as women appear to have suffered more than men from stay-at-home requirements, restrictions on private gatherings and school closures, while benefiting less from workplace closures.
Third, for some groups the average level of WHO-5 over the study period was already clearly below 13, the depression-risk threshold (WHO, 1998). These included women, people with non-tertiary education, those not living with a partner, and those living with children (below 18).
Policies may be needed to counteract the negative consequences of the pandemic itself and of the measures adopted to contain it, for instance by reducing the burden faced by women and individuals with young children, and to alleviate the resulting work-family conflict.
References
Douglas, M., Katikireddi, S.V., Taulbut, M., McKee, M., McCartney, G. (2020) Mitigating the wider health effects of COVID‒19 pandemic response. BMJ 369. Doi:10.1136/bmj.m1557
Eurofound (2016) European Quality of Life Survey 2016 (data set). (Accessed 20 April 2021).
Eurofound (2020). Living, working and COVID‒19, COVID‒19 series, Publications Office of the European Union, Luxembourg.
Hale, T., Webster, S., Petherick, A., Phillips, T., Kira, B. (2020) Oxford COVID‒19 government response tracker (OxCGRT), 8, p. 30.
Moreno, C., Wykes, T., Galderisi, S., et al. (2020) How mental health care should change as a consequence of the COVID‒19 pandemic. Lancet Psychiatr. Sep;7(9):813-824.
Santomauro, D.F., Herrera, A.M.M., Shadid, J., et al. (2021) Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID‒19 pandemic. Lancet.
Toffolutti, V., Plach, S., Maksimovic, T., Piccitto, G., Mascherini, M., Mencarini, L., Aassve, A. (2022) The association between COVID‒19 policy responses and mental well-being: Evidence from 28 European countries, Social Science & Medicine, doi: 10.1016/j.socscimed.2022.114906
WHO (1998) Well-being measures in primary health care/the DEPCARE project: report on a WHO meeting, Stockholm, Sweden 12‒13 February 1998. In: well-being Measures in Primary Health Care/the DEPCARE Project: Report on a WHO Meeting. Stockholm, Sweden 12‒13 February 1998.
WHO (2021) The Pandemic Paradox. (Accessed 2 November 2021).