Premature drops in estrogen from early menopausal age may increase the risk of disease and death in later life. To understand what influences early menopausal onset, we looked at the life course and sociodemographic factors at younger ages in Ugandan women aged 40-49. What they most need to reduce the risk of early menopause is improved contraception and education.
Background
Menopause is more than just a collection of unpleasant symptoms, such as hot flashes and brain fogs. The age when menstruation stops for good is an important marker for the woman’s future life and health. There is evidence that women reporting early menopause (before the global median age of 50), because of the drop in estrogen, are exposed to higher risks of heart and bone diseases (Golezar et al., 2019; Zhang et al., 2019) and of death (Shuster et al., 2010).
The age at menopause (conventionally starting twelve months after the last menstruation) does not occur at random: it hinges on biocultural experiences of reproduction in adolescence and throughout childbearing years, with effects that accumulate over time (Mishra et al., 2010; Leidy Sievert et al., 2013). The phenomenon has been frequently studied in low-fertility countries, but much less in a high-fertility setting (for an exception, see OlaOlorun & Lawoyin, 2009).
Research approach
In a recent article (Batista et al., 2022), we explored the combinations of individual characteristics and social circumstances that were conducive to menopause appearing between ages 40 and 49 among ever-married heterosexual Ugandan women, using data from the 2016 Demographic and Health Survey (Uganda Bureau of Statistics & ICF International Inc., 2018).
Women were asked numerous questions about their reproductive experiences, but the main factors that we explored were:
(a) if they ever used any method of modern or traditional contraception,
(b) the age when they gave birth to their first child, and
(c) how many children they gave birth to.
We expected reproductive factors to interact not only with each other, but also with sociodemographic factors such as education, wealth, rural-urban residence, marital status, and age at first marriage.
Main findings
About 17% of forty-year-olds in Uganda reported having experienced menopause when the survey was conducted in 2016. We studied their life course and found that never using contraceptives, having fewer children, and younger ages at first birth and marriage were associated with higher probabilities of menopause at ages 40-49.
In the pathways most likely to give rise to early menopause among Ugandan women, we found evidence of two interactive dynamics clustering around contraception. One emerged when no contraceptive use was linked to young age at first birth (Figure 1); the other, when lack of contraceptive use was linked to lack of education (Figure 2).
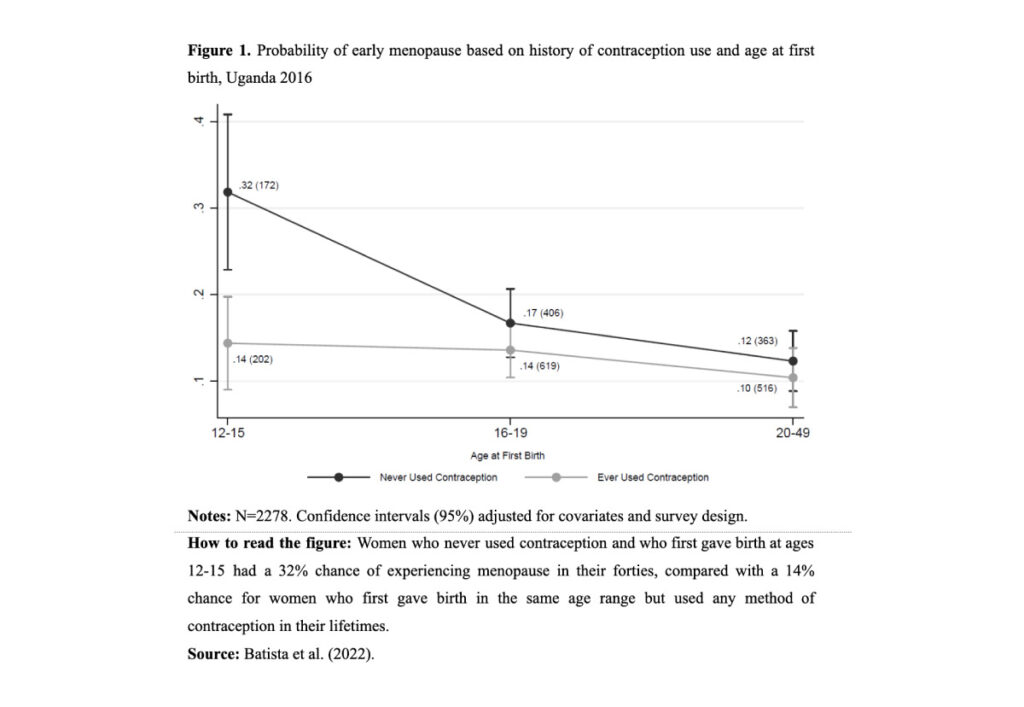
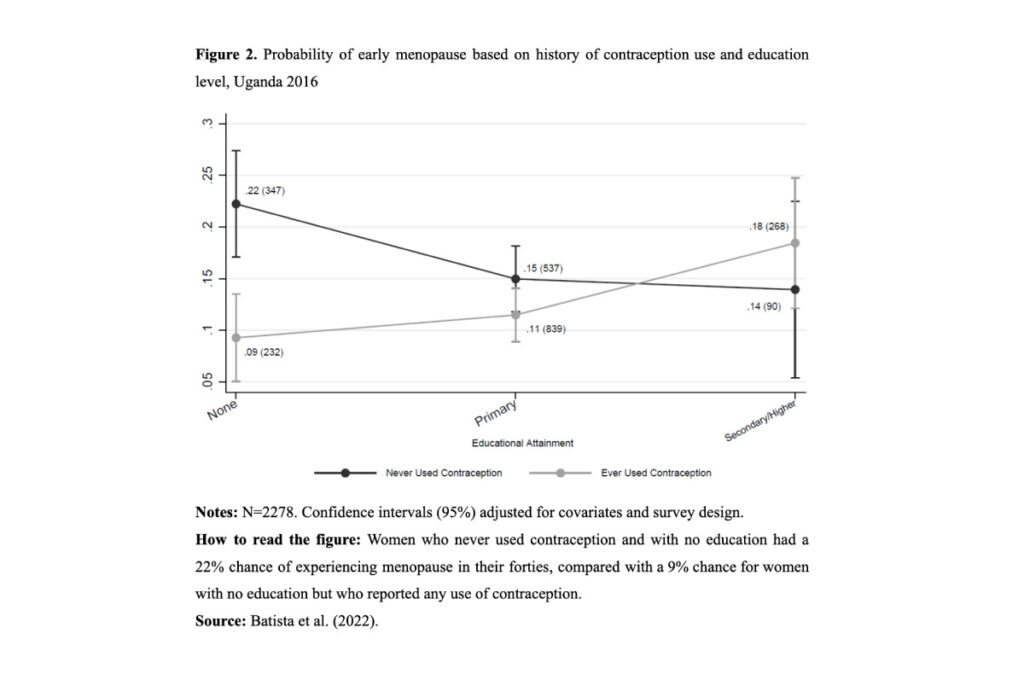
Early menopause has thus far been studied almost exclusively in low-fertility, high income countries. Therefore, scholars have typically identified different types of risk factors, such as childlessness or smoking cigarettes. None of these applies to Uganda, given the very low occurrence of both: only 1.5% of the sample reported either. What seems to matter there is a different set of underlying causes, such as young age at motherhood and lack of education.
Conclusions
Menopause typically receives less attention in women’s health research than other reproductive issues, especially among African women. The early onset of menopause, i.e., before the global median age of 50 years, should become a policy concern, because of its connection to higher morbidity and mortality in older years.
Increasing access to education for girls is better poised to increase menopausal age than simply increasing contraceptive use. Besides, increasing contraception would be most helpful in preventing early menopause for women with no education. For other women, reducing child marriage and delaying age at first birth seem to be more promising paths. These measures, which rank high in the comprehensive efforts already underway to improve women’s overall reproductive health, are also likely to result in older menopausal age.
References
Batista, M. S., Tsitsiou, Y., Dar, S., Ancillotti, G., Minhas, S., & Varshney, N. (2022). Life course reproductive dynamics associated with menopause in Ugandan women aged 40–49. American Journal of Human Biology. https://doi.org/10.1002/ajhb.23791
Golezar, S., Ramezani Tehrani, F., Khazaei, S., Ebadi, A., & Keshavarz, Z. (2019). The global prevalence of primary ovarian insufficiency and early menopause: A meta-analysis. Climacteric, 22(4), 403–411. https://doi.org/10.1080/13697137.2019.1574738
Leidy Sievert, L., Murphy, L., Morrison, L. A., Reza, A. M., & Brown, D. E. (2013). Age at menopause and determinants of hysterectomy and menopause in a multi-ethnic community: The Hilo Women’s Health Study. Maturitas, 76(4), Article 4. https://doi.org/10.1016/j.maturitas.2013.08.007
Mishra, G. D., Cooper, R., & Kuh, D. (2010). A life course approach to reproductive health: Theory and methods. Maturitas, 65(2), 92–97. https://doi.org/10.1016/j.maturitas.2009.12.009
OlaOlorun, F., & Lawoyin, T. (2009). Age at menopause and factors associated with attainment of menopause in an urban community in Ibadan, Nigeria. Climacteric, 12(4), 352–363. https://doi.org/10.1080/13697130802521282
Shuster, L. T., Rhodes, D. J., Gostout, B. S., Grossardt, B. R., & Rocca, W. A. (2010). Premature menopause or early menopause: Long-term health consequences. Maturitas, 65(2), Article 2. https://doi.org/10.1016/j.maturitas.2009.08.003
Uganda Bureau of Statistics & ICF International Inc. (2018). Uganda Demographic and Health Survey 2016.
Zhang, X., Liu, L., Song, F., Song, Y., & Dai, H. (2019). Ages at menarche and menopause, and mortality among postmenopausal women. Maturitas, 130, 50–56. https://doi.org/10.1016/j.maturitas.2019.10.009