The fertility-contraceptive relationship has weakened in recent years, meaning that greater contraceptive prevalence is needed to obtain a comparable reduction in fertility. Various explanations have been attempted, including unobserved heterogeneity and greater use of less effective methods. Yoonjoung Choi, Madeleine Short Fabic and Jacob Adetunji offer a different perspective: the age distribution of users (usually ignored in the study of contraception) does not match that of the population at risk (women of reproductive age).
Introduction
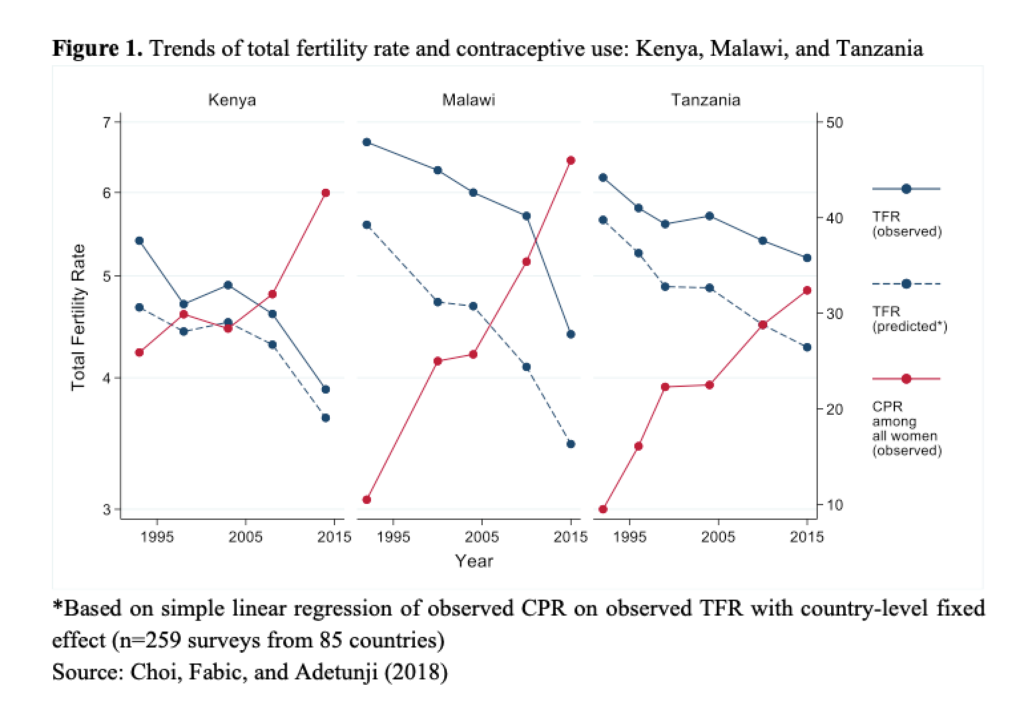
The association between contraception and fertility is one of the strongest among all the proximate determinants of fertility: every 15 percentage-point increase in the contraceptive prevalence rate (CPR) is associated with a reduction of 1 in the total fertility rate (TFR) (Mauldin and Segal 2015; Ross and Frankenberg 1993; Tsui 2001). Over the last decade, however, this relationship appears to have weakened. Impressive increases in contraceptive prevalence in a number of countries have met with less than expected declines in total fertility. Take Tanzania, for example, where CPR among all women has steadily increased. From Tanzania’s first Demographic and Health Survey in 1991 through its most recent in 2016, CPR increased from 10% to 32%, but TFR declined by only 1 (6.2 to 5.2) (Figure 1). Other countries in sub-Saharan Africa have also experienced rapid increases in CPR without commensurate declines in TFR.
Perplexed, a number of demographers have recently explored potential reasons for the diminishing association between CPR and TFR, such as unobserved heterogeneity (Bongaarts 2015; Stover and Winfrey 2017) and shifts in method mix towards less effective methods (Bertrand et al. 2014; Ross et al. 2015; Zheng et al. 2012).
Measurement mismatch?
One factor that has not received as much attention is related to measurement mismatch. While TFR and CPR are both population-level measures, TFR is a synthetic cohort measure that is age-adjusted (it is calculated for different age groups and then aggregated), but CPR is not age-adjusted (it is calculated across all age groups combined). There are two major reasons why this age-adjustment ‘mismatch’ may now matter:
- Changing age patterns of contraceptive use: Women’s physiological ability to have children declines over their reproductive years. Increased contraceptive use will reduce fertility by a smaller magnitude among women of older ages than among women of younger ages. When rapid increases in contraceptive use are more concentrated among older women, we would expect the TFR-CPR relationship to be attenuated.
- Changing population age structure: The population pyramids of low-income and lower-middle-income countries were quite similar 30 years ago. Over the intervening years, the population age distribution has remained relatively stable in low-income countries but has shifted significantly in lower-middle-income countries to increasingly reflect the distribution of high-income countries. With changing age structures, a contraceptive use measure that is not age-adjusted may be limited when comparing trends within a country as well as across countries.
We explore the measurement mismatch factor in our recent research (Choi, Fabic, and Adetunji 2018), which aims to a) assess whether the associations between TFR and CPR have indeed changed over time; and b) examine whether the TFR-CPR relationship is stronger when we use an age-adjusted CPR measure. Our analyses employ Demographic and Health Surveys data from 259 surveys conducted in 85 countries (DHS Program API).
Associations between TFR and CPR have indeed changed
We explore associations between TFR and CPR in two periods: 1985–2000 and 2001–2016. A TFR decrease of 1 is associated with a CPR increase of 15 percentage points in the earlier period and 17 percentage points in the later period. Additionally, CPR explains substantially less variation in TFR during the later period compared to the earlier period. When we restrict the analysis to surveys conducted in sub-Saharan Africa, where recent data motivated this study, we find that a TFR decrease of 1 percentage point is associated with a CPR increase of 18 percentage points during the 1985–2000 period and of as many as 20 percentage points later on, in 2001–2016.
Age-adjusted CPR better explains the association between contraceptive use and TFR.
Following the synthetic cohort approach used for TFR calculation, we calculate age-adjusted CPR among all women of reproductive age. This is a synthetic measure of the percentage of women ages 15– 49 years who would be using a contraceptive method if they were to go through their childbearing years using contraception according to the current schedule of five-year age-group-specific contraceptive prevalence rates in their country. When we compare the linear relationships between TFR and CPR—using both the unadjusted and age-adjusted measure—we find that age-adjusted CPR better explains the variance in fertility data.
Examples from Dominican Republic and Egypt show how age-adjusted and unadjusted CPR can differ due to age patterns of contraceptive use and population age structure (Figure 2).
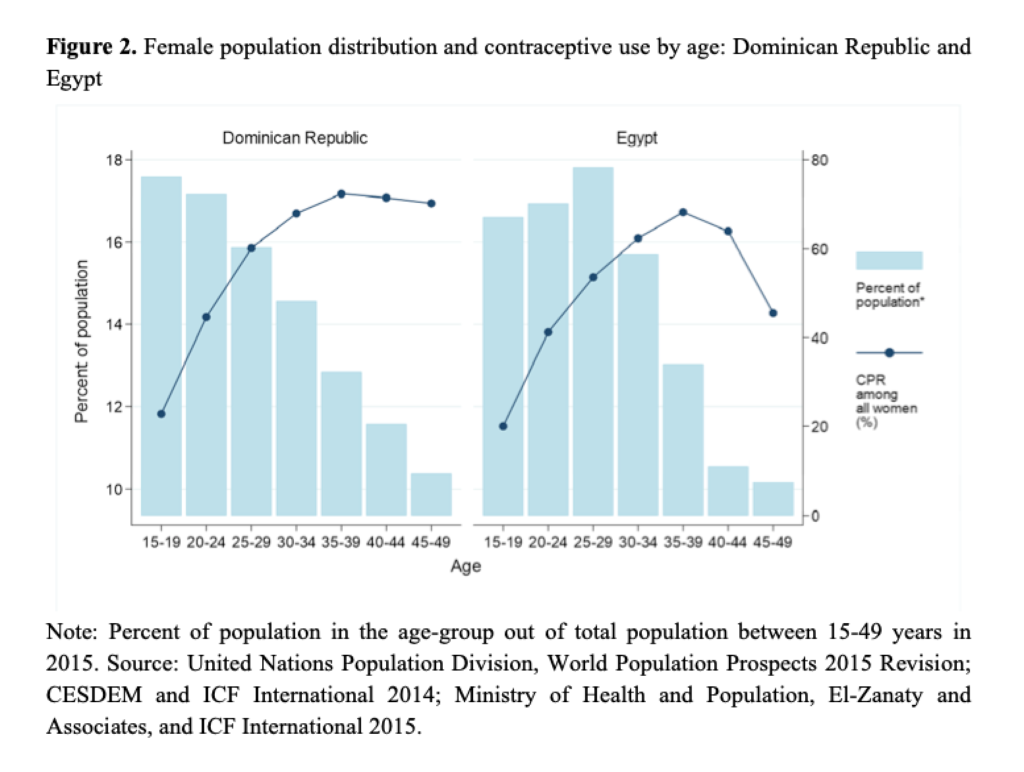
While both countries have unadjusted CPR of 55%, age-adjusted CPR is higher in the Dominican Republic (59%) and lower in Egypt (51%). In the Dominican Republic, women aged 15–19 constitute the largest proportion of all 15–49-year-old women, which means that unadjusted CPR is more weighted by younger women, who are also the subset of women in the country least likely to use contraception. Thus, unadjusted CPR is lower than age-adjusted CPR. Conversely in Egypt, women aged 25–29 account for a larger proportion of all women of reproductive age. Because these women are already more likely to use contraception than their younger counterparts, unadjusted CPR is higher than age-adjusted CPR.
So what?
First, we need to update our demographic shorthand for describing the TFR-CPR association. It used to be that an increase of 15 percentage points in CPR was associated with a reduction of 1 in TFR; now it is 17 percentage points. In sub-Saharan Africa, we should expect to see an increase in CPR of at least 20 percentage points before we see a reduction of 1 in TFR.
Second, our study highlights the importance of demographic considerations—age patterns of contraceptive use and population age structure—when assessing the impact of contraception on fertility trends over time. Using an age-adjusted measure of contraceptive prevalence allows us to incorporate these demographic considerations in our analyses.
References
Bertrand, J.T., Sullivan, T.M., Knowles, E.A., Zeeshan, M.F., and Shelton, J.D. (2014). Contraceptive method skew and shifts in method mix in low- and middle-income countries. International Perspectives on Sexual and Reproductive Health 40(3): 144–153. doi:10.1363/4014414.
Bongaarts, J. (2015). Modeling the fertility impact of the proximate determinants: Time for a tune-up. Demographic Research 33(19): 535–560. doi:10.4054/DemRes. 2015.33.19.
Choi, Y., Fabic, M.S., and Adetunji, J. (2018) Does age-adjusted measurement of contraceptive use better explain the relationship between fertility and contraception? Demographic Research 39(45):1227-1240. DOI: 10.4054/DemRes.2018.39.45.
CESDEM and ICF International (2014). Republica Dominicana encuesta demografica y de salud 2013. Santo Domingo: Centro de Estudios Sociales y Demograficos and ICF International.
Mauldin, W.P. and Segal, S.J. (1988). Prevalence of contraceptive use: Trends and issues. Studies in Family Planning 19(6 Pt 1): 335–353. doi:10.2307/1966628.
Ministry of Health and Population, El-Zanaty, F. and Associates, and ICF International (2015). Egypt demographic and health survey 2014. Cairo: Ministry of Health and Population and ICF International.
Ross, J., Keesbury, J., and Hardee, K. (2015). Trends in the contraceptive method mix in low- and middle-income countries: Analysis using a new ‘average deviation’ measure. Global Health: Science and Practice 3(1): 34–55. doi:10.9745/GHSPD-14-00199.
Ross, J. and Frankenberg, E. (1993). Findings from two decades of family planning research. New York: Population Council.
Stover, J. and Winfrey, W. (2017). The effects of family planning and other factors on fertility, abortion, miscarriage, and stillbirths in the spectrum model. BMC Public Health 17(S4): 775. doi:10.1186/s12889-017-4740-7.
Tsui, A.O. (2001). Population policies, family planning programs, and fertility: The record. Population and Development Review 27(Supplement: Global Fertility Transition): 184–204.
Zheng, X., Tan, L., Ren, Q., Cui, Z., Wu, J., Lin, T., He, J., and Chen, H. (2012). Trends in contraceptive patterns and behaviors during a period of fertility transition in China: 1988–2006. Contraception 86(3): 204–213. doi:10.1016/j. contraception.2011.12.006.
*Views and opinions expressed are the authors’ and do not represent the views or opinions of USAID