Advanced maternal age and low birth weight

The negative association between advanced maternal age and low birth weight has become progressively weaker over time in the UK (between 1958-2001). This pattern, as Alice Goisis explains, is partly linked to secular changes in the characteristics of older mothers.
Existing studies provide contradictory evidence on the association between advanced maternal age and child health, with some studies finding a negative association and others a lack of one (Bewley, Davies and Braude 2005; Carolan and Frankowska 2011; Cunningham and Leveno 1995). One potential reason for the lack of general consensus about the risks associated with giving birth at an advanced maternal age is that these associations might be changing over time. Mothers who give birth at an advanced age today could be facing lower risks of poor neonatal outcomes than their counterparts in the past (Carolan 2003). Secular changes may have occurred because of changes in the characteristics of older mothers, and due to improvements in medical and obstetric practices. Up to now, however, no study has analysed whether this is the case, despite the increasing proportion of women giving birth at advanced maternal ages.
Data and variables
A recent study (Goisis, Schneider, and Myrskylä 2018) used data from four large UK birth cohort studies covering births that occurred in the UK between 1958 and 2002: the 1958 National Child Development Study (NCDS), the 1970 British Cohort Study (BCS), the 1992 Avon Longitudinal Study of Parents and Children (ALSPAC), the 2000-2002 Millennium Cohort Study (MCS).
The outcome is a binary variable indicating whether the cohort child was low birth weight (or LBW), defined as having a birth weight below 2.5 kg. Mothers’ ages at birth were divided into six categories: under 20 (<20), 20–24, 25–29, 30–34, 35–39, and 40 or older (40+). We define advanced maternal age as ages 40+, as previous work has shown that the association between advanced maternal age and adverse birth outcomes becomes clinically relevant after this age threshold (Mills and Lavender 2011).
Have the characteristics of older mothers changed over time?
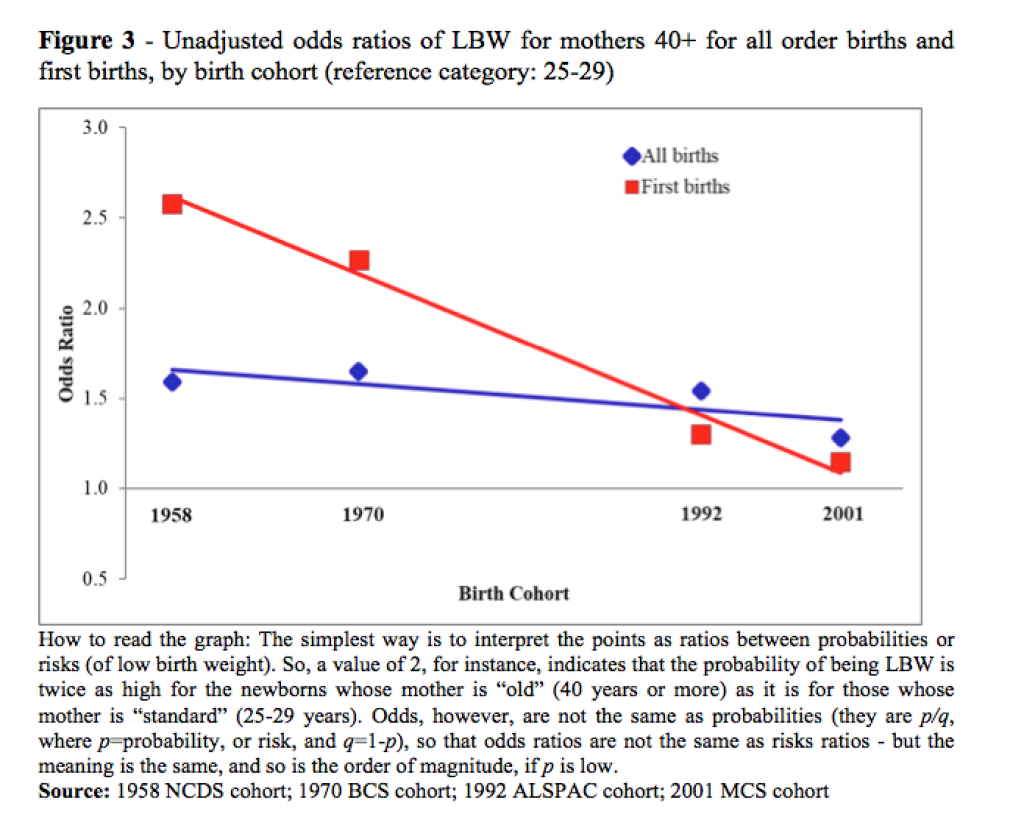
Across the cohorts, older mothers became progressively more advantaged than younger mothers. In particular, the differences in the profiles of mothers who gave birth at age 40+ and those who gave birth in their 20s became larger and advanced maternal age became increasingly associated with socio-economic advantage and good health behaviours. For example, Figure 1 shows that amongst mothers who gave birth in 1958 or 1970 there was a smaller percentage of mothers who gave birth at advanced maternal ages in a high social class group than mothers who gave birth in their mid-20s. In contrast, amongst women who gave birth around 1992 or 2001, we observed the opposite pattern, with older women being more likely to belong to the high social class group than younger ones. Figure 2 shows that there was virtually no age gradient in smoking during pregnancy in 1958 and 1970, whilst amongst mothers who gave birth around 1992 or 2001 older mothers were less likely to smoke during pregnancy than younger mothers.
Has the association between advanced maternal age and LBW changed over time?
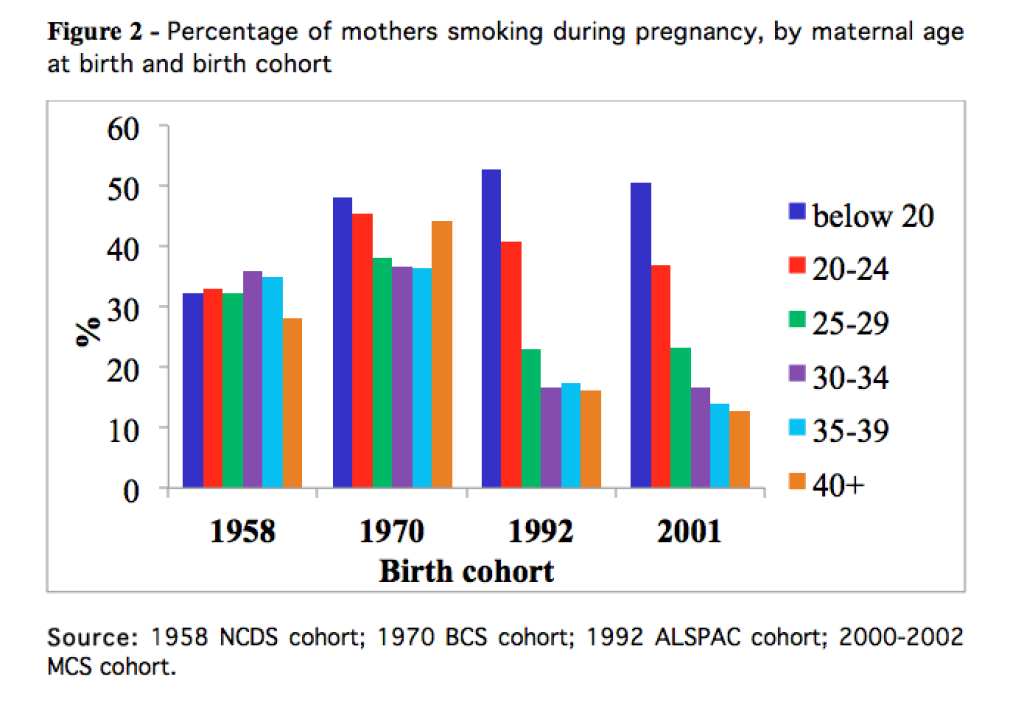
Figure 3 shows the unadjusted odds ratios of low birth weight associated with giving birth at ages 40+ across the different cohort studies for all births and for first births only. The reference category was mothers who gave birth at ages 25-29. The results show that giving birth at advanced maternal ages became less likely to be associated with LBW across the cohorts – in particular when we compared the least to the most recent cohort. The secular decline in the negative association between advanced maternal age and LBW was more pronounced for first births. The adjustment in the model for mothers’ characteristics was useful to explain the secular trends. In particular, only in the most recent cohorts did the adjustment for mothers’ socio-demographic characteristics (e.g. education, social class, marital status) increase the odds of LBW associated with advanced maternal age to a level similar to that observed in the unadjusted model for 1958/1970. This suggests that the fact that older mothers have become progressively more advantaged over time constitutes an important mechanism explaining why older mothers today face lower risks of LBW than older mothers in the past. We were not able to test for the role of changes in the medical context. Nonetheless, the cross-cohort differences in the fully adjusted model could suggest that access to modern obstetric care has modified and reduced the risks associated with giving birth at advanced maternal age.
Conclusion
The study shows that in the UK the association between advanced maternal age and child health has not remained constant over time and is tied to the time period under consideration. Across successive birth cohorts, the association between advanced maternal age and LBW has weakened, and has become negligible for the most recent birth cohorts. The decline in the association is at least partially explained by the socio-economic advantages of older mothers in the most recent cohort studies.
References
Bewley, S., M. Davies, and P. Braude. 2005. “Which career first? The most secure age for childbearing remains 20-35.” British Medical Journal 331:588-589
Carolan, M. 2003. “The graying of the obstetric population: Implications for the older mother.” Journal of Obstetric Gynecologic and Neonatal Nursing 32(1):19-27.
Carolan, M.and D. Frankowska. 2011. “Advanced maternal age and adverse perinatal outcome: A review of the evidence.” Midwifery 27(6):793-801.
Cunningham, F.G.and K.J. Leveno. 1995. “Childbearing among Older Women — The Message is Cautiously Optimistic.” New England Journal of Medicine 333(15):1002-1004.
Goisis, A., S.D. Schneider, and M. Myrskylä. 2018. ” Secular changes in the association between advanced maternal age and the risk of low birth weight: a cross-cohort comparison in the UK.” Population Studies.
Mills, T.A.and T. Lavender. 2011. “Advanced maternal age.” Obstetrics, Gynaecology & Reproductive Medicine 21(4):107-111.